Limb Lengthening and Reconstruction
Written by
Dr. Tim O'CARRIGAN
FRACS., FA OrthoA.
Click here for printable handouts on Limb Lengthening & Reconstruction.
Decision making in Limb Lengthening and Reconstruction
Limb lengthening and reconstruction techniques can be used to replace missing bone and to lengthen and/or straighten deformed bone segments. These procedures may be performed in both children and adults who have limb length discrepancies due to birth defects, disease, or injury.
The limb lengthening and deformity correction process works on the principle of distraction osteogenesis. This is a revolutionary concept, reversing the long-held belief that bone could not be regenerated. With this process, a bone that has been cut during surgery is gradually distracted (pulled apart), leading to new bone formation (osteogenesis) at the site of the lengthening. In this way, bone segments can be lengthened by 15 to 100% of their original length.
 Who was Ilizarov?
Who was Ilizarov?
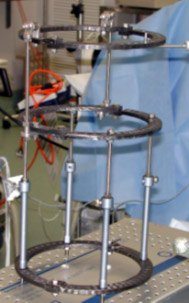
In 1951, Professor Gavril Abramovich Ilizarov from Kurgan in the Soviet Union developed a circular external fixateur for the treatment of fractures. During the next decade, Ilizarov discovered many techniques, including physeal distraction, corticotomy lengthening, and bone transport. He called the common basis for all of these methods the theory of tension stress. Through controlled, mechanically applied tension stress, Ilizarov was able to show that bone and soft tissue can be made to regenerate in a reliable and reproducible manner. During the next 41 years, until his death in 1992 at the age of 71, he developed countless clinical applications of bone and soft tissue regeneration.
Where did i Train?
I did a twelve month fellowship at the International Center for Limb Lengthening in Baltimore Maryland USA (www.mcllr.com) This is the most experienced centre for limb lengthening and reconstruction in the United States and is run by Drs Dror Paley and John Herzenberg who are the two foremost Ilizarov surgeons in America . Comprehensive instruction in all aspects of limb lengthening and reconstruction was undertaken. There are no other surgeons in New South Wales and only one other surgeon in Australia who has undertaken as extensive formal training in limb reconstruction surgery.
Indications
- Leg Length Discrepancy
- Post - Traumatic Bone Deformities
- Nonunions
- Malunions
- Bone Loss
- Joint Contractures
- Osteomyelitis
Leg Length Discrepancy
Leg length discrepancy (LLD) results from congenital, developmental, posttraumatic, or post-surgical causes.
Posttraumatic LLD occurs after fractures when bones heal in a shortened position.
Treatment goals are correction of LLD with associated deformity while preserving function of muscles and joints and restoring normal alignment of the limb.
This patient corrects for her leg length discrepancy by tilting her pelvis

Post - Traumatic Bone Deformities
Posttraumatic bone deformities are fractures that heal in a displaced, angulated, rotated, or shortened position

Non-Healing Fractures (nonunions) and Malunions
Fractures that do not heal result in nonunions. These may be associated with limb length discrepancy, infection, and stiff joints.
Fractures can heal in an incorrect position with shortening, angulation or rotation. This is called a malunion.
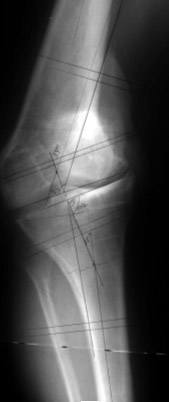
 This is a non-union
This is a non-union
Bone Loss from Tumour, Trauma or Infection
Tumour, trauma, and infection can all lead to bone loss due to either the injury or resection. Bone loss may be manifested as a bone defect or as limb length discrepancy or both.
Joint Contractures
Joints may be limited in their movement from tight muscles or capsule or from scarring in the joint.
Bone Infection (Osteomyelitis)
Bone infection may be a result of fracture or blood borne infection (usually occur during childhood).
Usually the only way to effectively eradicate established bone infection is to resect the abnormal bone and this can result in a bone defect that needs to be reconstructed using the Ilizarov technique.


The Process
Phase 1: Consultation
The initial assessment involves detailed history examination and review of previous x-rays. Specialized x-rays are usually required to complete the assessment. The initial assessment and discussion often takes an hour.
If surgical treatment is considered appropriate, all aspects of the procedure are discussed with the patient. The patient is encouraged to consider the information and a follow up appointment is made to answer any further questions and make definitive treatment plans.
It is extremely important that the patient and the surgeon have a clear understanding of the goals of surgery. It is important the patient understands what can realistically be achieved by the surgery and the potential complications both common and minor and rare but serious.




Phase 2: Surgery
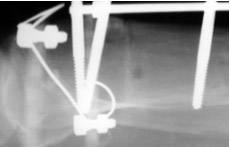
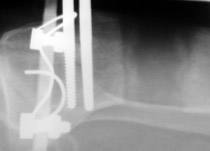
The surgeon in preparation for each surgery preconstructs a customized apparatus. Using wires or pins, the apparatus is surgically attached to the affected limb. Surgery is usually performed percutaneously through small incisions. Special care is taken to minimize injury to the bone and surrounding soft tissue, nerves and blood vessels when making specialized bone cuts.
Phase 3: Postoperative Treatment and Rehabilitation
Adjustment Phase
Generally, patients remain in the hospital for 3 to 7 days before they are discharged home. A more complex procedure may require a longer inpatient stay.
The actual lengthening or straightening of the limb begins 1-2 weeks after surgery. At that time, adjustments are made to the apparatus usually four times a day. Detailed instructions are provided to the patient to ensure they fully understand what is required.
The bone ends are separated at a rate of 1 mm per day.
Muscles do not lengthen as easily as bone and therefore physiotherapy may be an important part of the treatment to maintain joint range of motion and prevent contractures. A joint at risk may be included in the frame to prevent contractures that would otherwise occur.
Swimming and showering are allowed with the apparatus in place once initial wound healing has occurred at 5-7 days postoperatively.
During the adjustment phase the patient is followed up in the rooms every two weeks with clinical examination and x-rays. A close scrutiny is maintained to identify any complications early.
- Latent phase
for restoration of endosteal and periosteal blood vessels
- Distraction phase
1mm/day until desired length is achieved
- Consolidation phase
allows for intramembraneous ossification and recanalization of new bone

Consolidation Phase (Bone Hardening)
After the desired length has been achieved and the limb has been straightened, no further adjustments are made. The apparatus is left in place to allow the new bone to harden and mature. Once the new bone is judged to be sufficiently strong, the frame is removed under a short general anaesthetic. A cast or brace may be applied for an additional month or two for further protection. The new bone tissue assumes all the qualities and strength of normal bone with time.
During the adjustment phase the patient is seen every month.
Follow-Up
With close follow up if a problem is arising then it can be picked up early and can usually be treated without affecting the final outcome.
All the necessary surgeries are anticipated and communicated to the patient before treatment commences but sometimes an unscheduled operation is required to correct a problem.
When the desired correction is achieved the frame is locked down and the consolidation phase begins. The patient is seen on a monthly basis with x-rays and examination.
I am very conservative regarding when to remove the frame. This is to minimize the risk of deformation of the regenerate or fracture after frame removal, which can be a devastating complication. When it is thought that it is time to remove the frame then it is completely loosened so that it is not assisting in weight bearing and the patient is encouraged to fully weight bear for two weeks. If this can be achieved without any loss of correction then the frame removal is scheduled. If there is loss of position then usually this can be corrected by frame adjustment on an outpatient basis thereby avoiding needing further surgery.
Pain Relief
The adjustment phase is painful because of the constantly changing conditions for the bone and soft tissue. Standard pain medications often are not all that effective especially at night when sleep can be significantly disturbed. If a patient is not getting much sleep it does affect his/her ability to cope- as well as his/her carer. I often get patients to see a pain management specialist who can assist with appropriate medication. He is aware of all the side effects, interactions and appropriate dosages and therefore is best qualified to handle this aspect of your care. On occasions we arrange a pain specialist review before treatment commenences so a comprehensive pain management plan is in place.
Care of pin-sites
You are able to shower with an Ilizarov frame once the wounds are dry this is usually by day 5.
You should clean your pin sites once a day using an antibacterial solution such as Chlorhexidine 0.05%, using cotton wipes to wipe around each individual pin site in a circular motion. Sometimes a soft tooth brush may be required to clean up a build up of scab that often forms around the pin sites. This is quite normal as the body tries to heal its self.
Some people may experience a lot of ooze coming from a particular pin site, do not be alarmed as this can be quite normal. If this does occur soak a piece of lyofoam in the chlohexidine antibacterial wash, then place the lyofoam around the pin site. You may find that you need to change this dressing on a regular basis (some times 2-3 times a day).
If any of your pin sites start to looks red please seek medical attention from your local doctor or contact the rooms to seek further instructions from Dr O’Carrigan. As antibiotics maybe required. Once the pin sites have stopped oozing, and they look clean and dry they can remain uncovered.
Clothes modification
Skirts, pants, jeans, shorts: by splitting the seem on the affected side and attaching Velcro or press studs to the seem can make it a lot easier to dress.
Smoking
If you are suitable for this type of surgery and you are a smoker, than you have to stop smoking immediately as smoking affects bone growth and healing process. If you are not prepared to stop smoking than you will find that your Orthopedic surgeon will not carry out this procedure.
- Click here to open an printable document for pin-site care for patients with Ilizarov frame.
Complications
All surgery has the potential for complications and Ilizarov surgery is no exception. With careful preoperative planning and close co-operation between surgeon and patient and realistic treatment goals most complications can be avoided and a successful outcome achieved.
When a surgeon discusses a possible procedure with a patient he has to be a pessimist and talk about the worst-case scenario. That relates to the anaesthetic and the surgery itself.
Anaesthetic Complications
In the worst-case situation you can die under an anaesthetic or have a major stroke or heart attack that can be life threatening or have permanent consequences. Fortunately these events are very rare these days but the chances are increased if a patient has intercurrent illnesses such as diabetes or heart, lung problems.
The treatment of any intercurrent illnesses should be optimized prior to surgery and this may involve delaying the surgery until appropriate medical assessment has been performed usually with the assistance of your local doctor. It is important that you have a regular local doctor prior to commencing Ilizarov surgery because they can be an important resource to assist in the treatment phase in consultation with the surgeon.
Anaphylaxis
Very rarely a patient can be allergic to a medication that we are unaware of. That reaction can vary from a rash to a severe life threatening reaction called anaphylaxis.
Surgical Complications
These can vary from minor to severe and limb threatening.
Infection
Infection is a potential problem with any surgery. Deep infection in Ilizarov surgery is rare because most of the surgery is percutaneous . Pin tract infections however are common and most can be treated with careful pin tract cleaning and oral antibiotics. Rarely someone would require admission to hospital for debridement of a pin site and IV antibiotics or removal/ exchange of a pin or wire.
You are provided with information on pin site care in hospital and encouraged to shower using antimicrobial soap that you can obtain from your chemist.

DVT/Pulmonary Embolus
A DVT is a Deep Vein Thrombosis and this is a clot in the leg that can complicate any surgery. It can enlarge inside the leg and break off and travel to the lung where it is called a Pulmonary Embolus. It can make you very sick and if it is big enough you can die from it.
A number of precautions are taken in hospital to minimize the risk including a subcutaneous injection of a blood thinner called Clexane. Usually you are sent home with Clexane injections for two weeks and present to the first follow-up review with a Doppler Ultrasound test to ensure there is no evidence of a DVT. If this is clear then the Clexane is discontinued. If there is evidence of a DVT then the Clexane is continued until you are warfarinized which is a tablet that thins out your blood. This requires regular blood test and needs to be supervised by your local doctor in conjunction with a vascular physician.
Nerve/Blood Vessel Injury
Great care is taken to prevent injury to nerves or blood vessels during the surgery. All the structures at risk are kept in mind throughout the surgery. Despite this it is still possible to injure one of these structures. A nerve injury can vary from a temporary injury that recovers in days to weeks to normal function to a permanent partial or total loss of function of the nerve. This can cause permanent numbness and loss of joint movement and muscle power with wasting. The nerve most at risk is the sciatic nerve and its branches. Particularly the Peroneal nerve just below the knee.
Blood vessel injuries can cause significant blood loss or lead to ischaemia (loss of blood supply) to a limb that if not corrected will lead to loss of that limb. Fortunately both of these complications are extremely rare.
Premature Consolidation
The aim is to let the surgically induced fracture (osteotomy) to start to heal but then stretch (distract) it to lengthen and/or straighten the bone. Some people and some bones heal faster than others and it can get stuck which is called premature consolidation. If this occurs we can sometimes get it unstuck by continuing turns but other times it requires another short operation to recut the bone.
Nonunion
Poor new bone formation can occur and sometimes this can develop into a nonunion where the bone fails to heal. In this situation modification of the frame may be necessary and a bone graft may have to be taken from the pelvis to achieve bone union.
Malunion
Malunion is where the bone heals but in an unsatisfactory position. This is extremely rare in Ilizarov Surgery because we can adjust the frame and take x-rays until we are totally satisfied with the position and then lock down the frame. With a stable frame the position will not be lost. Sometimes late deformity can occur after removal of the frame.
Joint Contracture
Muscles and tendons don't lengthen as well as bone does and the limiting factor in how much we can lengthen a limb is muscle tightening and joint contracture. Sometimes a frame is extended across a joint to correct or prevent a contracture occurring. The joints most at risk a re the knee and the ankle.
Physiotherapy and stretching performed by the patient and sometimes formal physiotherapy are critical to a successful result. The soft tissues and joint range of motion are often the difference between a “good” result and a “great” result.
Sometimes surgical release of tight soft tissues is necessary.
Fracture/ Late Deformity
The decision about when to remove a frame is a difficult one. We don't want to keep it on longer than necessary but if you remove it too early then the new bone can fracture or deform. This can undo all the good work and is extremely frustrating for the surgeon and devastatingly disappointing to the patient.
When I judge that the frame is ready for removal then I loosen the frame right off and allow the patient to fully weight bear for two weeks and then review with repeat x-rays. If there is no pain and no loss of correction then the frame can be removed under a general anaesthetic and usually no post- removal cast of brace is necessary.
Fracture post frame removal requires surgical intervention usually in the form of an intramedullary nail.

Overlengthening or Underlengthening
This is possible but rare because with the Ilizarov method you can gradually correct the deformity until it is perfect and then lock down. For a week to two weeks you can make further fine adjustments except it is difficult to recommence lengthening after more than a few days of consolidation.
Scarring
Some scars are inevitable. They usually fade largely with time and do not create a significant cosmetic problem
Reflex Sympathetic Dystrophy(Complex Regional Pain Syndrome)
This is where the nerves react adversely to an operation or injury and become hypersensitive and hyper-reactive. It is characterized by excessively severe pain swelling and stiffness and hypersensitivity. The pain is usually not amenable to standard analgesics and pain management specialist review is necessary. Treatment usually consists of medication, nerve blocks and physiotherapy. The earlier it is picked up and treated the better it does. It is not possible to predict who this will happen to unless there is a previous history and despite treatment it can lead to permanent disability.
Loss of Function
Everything that limb deformity surgery is aiming to do is to relieve pain and restore function. Sometimes this is not achieved despite the best intentions because of complications that are an inherent risk with the surgery. It is possible for someone to be functionally worse off after surgery than they were before. This can occur with any surgery and is not restricted to limb lengthening and deformity correction.
Unplanned Return to Theatre
If a problem is identified then sometimes surgery is necessary to correct this problem so that is does not compromise the final result. The earlier and more aggressively a complication is treated then the better the outcome usually.
Amputation
One of the most devastating complications that can complicate limb deformity surgery is amputation. This can complicate any operation- even very simple surgery. Major nerve or blood vessel injury can necessitate amputation as can limb threatening infections such as gangrene. These complications are extremely rare but have been reported.
Conclusion
Correction of deformity with the Ilizarov Fixateur is a time consuming and challenging process for both the patient and the surgeon. It is also an extremely worthwhile process because it can make a tremendous improvement in a patient's pain, function, appearance and quality of life.
With clear realistic goals shared by both the surgeon and patient combined with patience and co-operation then the goals can be reliably achieved with the minimum of complications.
Dr Tim O'Carrigan MBBS FRACS
